Whenever our senior team participates in professional development workshops with GPs and allied health practitioners, we often hear “I don’t have any eating disorder patients”.
However, statistically speaking, a GP sees (either knowingly or unknowingly) at least 1 patient with an active eating disorder each day.
Eating disorders have the highest mortality and morbidity rates of all psychiatric illnesses with reports claiming that someone with an eating disorder dies every 52 minutes as a direct result of their illness.
However, in Australia, it is estimated that only 1 quarter of those with an eating disorder are known to a medical or allied health practitioner.
Continue reading for the top 3 reasons eating disorders get missed (and what to do about it).
1. The presenting complaint is not obvious.
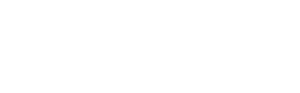
A patient with depression presents with a low mood, a patient with a possible brain tumour presents with a headache, however the patient with an eating disorder rarely presents with complaints about food or eating (if they do, it should be taken seriously).
For a host of different reasons, patients with an eating disorder don’t usually know that they have a problem. The most cited reasons that someone with an undiagnosed eating disorder presents to the GP include:
- Unexplained fatigue and/or lethargy
- Changes to their cognitive and/or executive functioning
- Menstrual abnormalities
- Fertility concerns
- Gastrointestinal concerns or digestive issues
- Suspected or reported food intolerances
- Vitamin and/or mineral deficiencies (most commonly Iron, Vitamin D, Vitamin B12)
- Syncope, presyncope
- Increased sensitivity to bruising
- Changes in or concerns about body weight
- Failure to thrive (ie., deviations from growth trajectory)
2. Stigma and misconceptions.
When we think of eating disorders, we still tend to think of someone who is young, female, Caucasian, and has a BMI within the “underweight range”.
While an “underweight” BMI is a red flag and should be treated as such, most patients presenting to specialist eating disorder clinics and/or being admitted medically for an eating disorder do not have an “underweight” BMI. In fact, a recent study found that more than a third of adolescents with a serious eating disorder had a premorbid BMI above the 85th centile.
Eating disorders can affect all people of all walks of life. You can’t tell whether someone has an eating disorder by simply looking at them. It is important that all patients who report or endorse concerns about eating and/or weight are considered as possibly having an eating disorder and assessed (or referred to a specialist for an assessment) accordingly.
3. They are highly comorbid.
It is estimated that up to 80% of individuals with an eating disorder also meet diagnostic criteria for another mental health concern.
While some psychiatric diagnoses (ie., ADHD, Autism, anxiety disorders) increase an individual’s vulnerability to eating disorder onset, the signs/symptoms of eating disorders often mimic other psychiatric conditions (that weren’t apparent premorbidly).
Given the mortality and morbidity of eating disorders, it is important that a thorough assessment by an eating disorder specialist is conducted in any and all events that an eating disorder is suspected – including situations in which the eating disorder is thought to be secondary to or of less concern than another psychiatric condition.
What to look out for: Screening for eating disorders.
There is a long list of factors that put someone at risk of an eating disorder (ie., low self-esteem, perfectionistic tendencies, trauma history, experiences of weight-based bullying, etc) however dieting and/or weight loss (intentional or unintentional) are the strongest predictors of eating disorder onset.
For this reason, we encourage you to consider adding the following screening questions (or variations of) to all intake forms and/or patient consultations:
- Have there been any changes to your diet or eating behaviours?
- Have there been any changes to the amounts/types of physical activity that you engage in?
- Have there been any changes to your body weight?
- For adults: What is your highest (non-pregnancy) adult weight vs your current weight?
- For children: How does your child’s current weight centile compare to their weight centile over time?
If a patient reports or endorses concerns with food, eating, or their body weight/shape, remember, “if you hear hoofs, think horses not zebras”.
Conducting a full medical assessment as per the statewide guidelines for the medical management of eating disorders (in children and in adults).
Learn more
For more information on screening for, assessing, managing, and or obtaining specialist support for a patient with an eating disorder, please feel free to contact our Client Care Coordinators on the enclosed details or consult the list of resources below:
- Request for an in-service training event from CFIH
- Eating Disorder Core Skills: eLearning for GPs
- RACGP Training For GPs
Full recovery from an eating disorder is possible however, it requires identification, accurate diagnosis, and specialist treatment.